| A B C D E F G H I J K L M N O P Q R S T U V W X Y Z # |
Antithrombin III Activity, Plasma
Test CodeATIII - NCMC
CPT Codes
85300
Preferred Specimen
1 mL plasma from Blue Top (3.2% Na Citrate)
Minimum Volume
Full blue top tube or 1.0 mL plasma frozen
Instructions
- It is imperative that the tube be completely filled to frosted line. The ratio of blood to anticoagulant is critical for valid coagulation results. If obtaining blood with a syringe, fill the light blue-top (sodium citrate) tube first.
- If patient is on heparin, specimen must be centrifuged and separated within 1 hour of draw.
- Heparin contaminated tube is not acceptable.
- Keep specimen anaerobic.
- Patients with an extremely high hematocrit may require special tubes before obtaining blood for coagulation testing. Please contact the lab for further information.
- Using a plastic transfer pipette, remove plasma and transfer to a properly labeled polypropylene tube
- Re-spin plasma
- Remove plasma using a plastic transfer pipette and transfer to a properly labeled polypropylene tube
- Freeze plastic tube
Specimen Stability
| Specimen Type | Temperature | Time |
| Whole blood Na Cit on heparin | Ambient | 1 hour |
| Whole blood Na Cit (unopen/unspun) | Ambient | 4 hours |
| Plasma Na Cit (open/spun) | Ambient | 4 hours |
| Plasma Na Cit double spun and separated | Frozen -20 C | 2 weeks |
Reject Criteria (Eg, hemolysis? Lipemia? Thaw/Other?)
- Clotted
- Serum received instead of Sodium Citrate plasma
- Specimen past stability
- Frozen plasma received thawed
- Underfilled or Overfilled, blood/anticoagulant ratio must be 9/1; Specimens must be between 90% -110% full
- Collected in a 3.8% Sodium Citrate tube instead of 3.2% Sodium Citrate tube
- Drawn in outdated/expired tube
- Hemolyzed, icteric, or lipemic sample
Methodology
Setup Schedule
Monday through Sunday; Continuously
Report Available
Same day
Reference Range
80-120%
Clinical Significance
Antithrombin (AT), or Heparin Cofactor I, is the major inhibitor of blood coagulation and is essential for effective heparin therapy. By inhibiting the coagulation proteases, especially thrombin, FXa and FIXa, AT prevents uncontrolled coagulation and thrombosis. Antithrombin deficiency is associated with a high risk of thromboembolic disorders.
The Antithrombin assay can be used to exclude or diagnose hereditary deficiency in patients with a tendency toward thromboembolism, in pre-operative stages, before prescription of oral contraceptives, DIC, nephritic syndromes, liver diseases and in therapy with heparin or antithrombin concentrates.
In addition to congenital AT III deficiency, decreased AT III activity can be seen in association with severe liver disease, nephrotic syndrome, disseminated intravascular coagulation and other disease states where consumption is increased. AT III activity may also be decreased in patients on heparin therapy.
The Antithrombin assay can be used to exclude or diagnose hereditary deficiency in patients with a tendency toward thromboembolism, in pre-operative stages, before prescription of oral contraceptives, DIC, nephritic syndromes, liver diseases and in therapy with heparin or antithrombin concentrates.
In addition to congenital AT III deficiency, decreased AT III activity can be seen in association with severe liver disease, nephrotic syndrome, disseminated intravascular coagulation and other disease states where consumption is increased. AT III activity may also be decreased in patients on heparin therapy.
Performing Laboratory
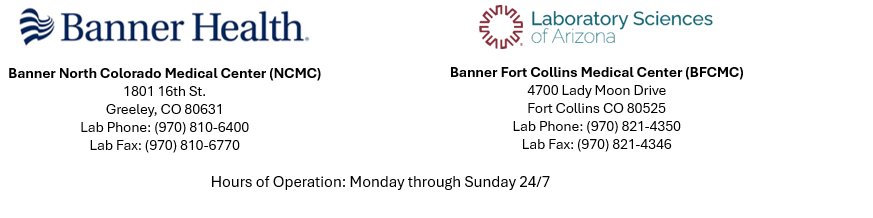
North Colorado Medical Center Laboratory