| A B C D E F G H I J K L M N O P Q R S T U V W X Y Z # |
Heparin, Low Molecular Weight, Anti Factor Xa
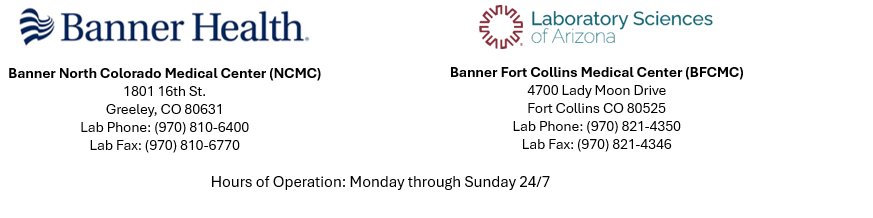
MessageSee specimen stability for guidance when drawing specimens at a location other than NLMC, North Colorado Medical Center, or Banner Fort Collins Medical Center. STAT courier must be called for transport to the performing laboratory when stability is less than 24 hours.
Test Code
LMWH - NCMC
CPT Codes
85520
Preferred Specimen
3.2% sodium citrate tube -blue top tube
Instructions
Light blue capped tubes (3.2% buffered sodium citrate) used for coagulation testing must be allowed to fill completely (after filling a small air space will normally be present). Short filled tubes will be rejected. Centrifuge within 1 hour of collection. Complete testing within 4 hours of collection or transfer specimen to polypropylene plastic tube using a plastic transfer pipette. Freeze plasma < -20°C.
Transport Temperature
Frozen
Specimen Stability
| · 4 hours at 2-8°C or 20°C, |
| · 2 weeks at -20°C |
Reject Criteria (Eg, hemolysis? Lipemia? Thaw/Other?)
| · clotted specimens |
| · underfilled or overfilled tube |
| · collection in 3.8% Citrate |
| · specimens collected in expired tubes |
| · serum samples |
| · specimen past stability |
| · thawed frozen samples |
| · Hemolyzed, icteric, or lipemic sample |
Setup Schedule
Monday through Sunday; Continuously
Report Available
Same Day
Reference Range
Therapeutic range for low molecular weight heparin varies with the brand and manufacturer, but is typically between 0.6-1.00 IU/mL.
Critical value (automatic call-back): >1.5 IU/mL
Note: Major institutions have shown that the most common reason for a sub therapeutic level is specimen not drawn at the proper time (4 hours post injection).
Critical value (automatic call-back): >1.5 IU/mL
Note: Major institutions have shown that the most common reason for a sub therapeutic level is specimen not drawn at the proper time (4 hours post injection).
Clinical Significance
Unfractionated Heparin (UFH) and Low molecular weight heparins (LMWH) are used for the prevention and treatment of thromboembolic diseases. The quantitative determination of plasma UFH and LMWH levels are useful for monitoring treatment efficacy.
Performing Laboratory
North Colorado Medical Center Laboratory