| A B C D E F G H I J K L M N O P Q R S T U V W X Y Z # |
Prothrombin Time (PT), Plasma
Test CodePT - NOCO
Alias/See Also
Protime
PT
INR
PT
INR
CPT Codes
85610
Preferred Specimen
1.0 mL plasma from Blue Top (Na Citrate)
Patient Preparation
- The patient's heparin drip should be paused for 1-5 minutes prior to collection, but should not exceed 5 minutes.
- Only use a discard tube if using a butterfly for specimen collection, then discard the first 3-5mL.
Minimum Volume
Full blue top tube or 1.0 mL plasma frozen
Instructions
- It is imperative that the tube be completely filled to frosted line. The ratio of blood to anticoagulant is critical for valid coagulation results. If obtaining blood with a syringe, fill the light blue-top (sodium citrate) tube first.
- If patient is on heparin, specimen must be centrifuged and separated within 1 hour of draw.
- Heparin contaminated tube is not acceptable.
- Keep specimen anaerobic.
- Patients with an extremely high hematocrit may require special tubes before obtaining blood for coagulation testing. Please contact the lab for further information.
- If testing will not be completed within 4 hours, spin down, remove plasma, and spin plasma again, and send specimen frozen in plastic vial.
- The light blue capped tubes, containing 3.2% buffered sodium citrate, used for coagulation testing must be allowed to fill completely (after filling a small air space will normally be present). For patients having a hematocrit greater than 55%, contact the hospital coagulation department to obtain a special collection tube.
Specimen Stability
| Specimen Type | Temperature | Time |
| Whole blood Na Cit on heparin | Ambient | 1 hour |
| Whole blood Na Cit (unopen/unspun) | Ambient | 24 hours |
| Plasma Na Cit (open/spun) | Ambient | 24 hours |
| Plasma Na Cit double spun and separated | Frozen -20 C | 2 weeks |
Reject Criteria (Eg, hemolysis? Lipemia? Thaw/Other?)
Clotted
Serum received instead of Sodium Citrate plasma
Specimen past stability
Frozen plasma received thawed
Underfilled or Overfilled, blood/anticoagulant ratio must be 9/1; specimens must be between 90% -110% full
Collected in a 3.8% Sodium Citrate tube instead of 3.2% Sodium Citrate tube
Drawn in outdated/expired tube
HCT > 55%
Hemolyzed, icteric, or lipemic sample
Samples received on ice
Serum received instead of Sodium Citrate plasma
Specimen past stability
Frozen plasma received thawed
Underfilled or Overfilled, blood/anticoagulant ratio must be 9/1; specimens must be between 90% -110% full
Collected in a 3.8% Sodium Citrate tube instead of 3.2% Sodium Citrate tube
Drawn in outdated/expired tube
HCT > 55%
Hemolyzed, icteric, or lipemic sample
Samples received on ice
Methodology
Setup Schedule
Monday through Sunday; Continuously
Report Available
Daily
Reference Range
System Standard (excluding Page)
Units of Measure = Seconds
Age Range: 0 - 150Y
PT 9.4 – 12.5
INR 0.9 - 1.1
AMR 8.0 - 150.0
Critical Range: INR >5.0
No anticoagulant Coumadin Therapy:
INR 2.0 - 3.0
Units of Measure = Seconds
Age Range: 0 - 150Y
PT 9.4 – 12.5
INR 0.9 - 1.1
AMR 8.0 - 150.0
Critical Range: INR >5.0
No anticoagulant Coumadin Therapy:
INR 2.0 - 3.0
Performing Laboratory
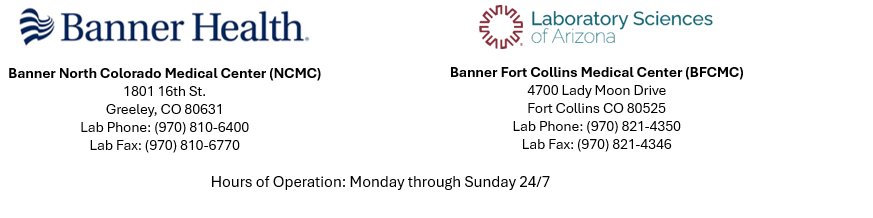
Banner Fort Collins Medical Center Laboratory
North Colorado Medical Center Laboratory